 – BY FACIAL PLASTIC SURGEON DR. HEATHER LEE
– BY FACIAL PLASTIC SURGEON DR. HEATHER LEE
Skin cancer is one of the most common malignancies, affecting 1 in 5 Americans in their lifetime. Unfortunately, the number of new cases has only continued to increase over the past decades.
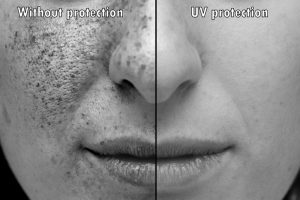
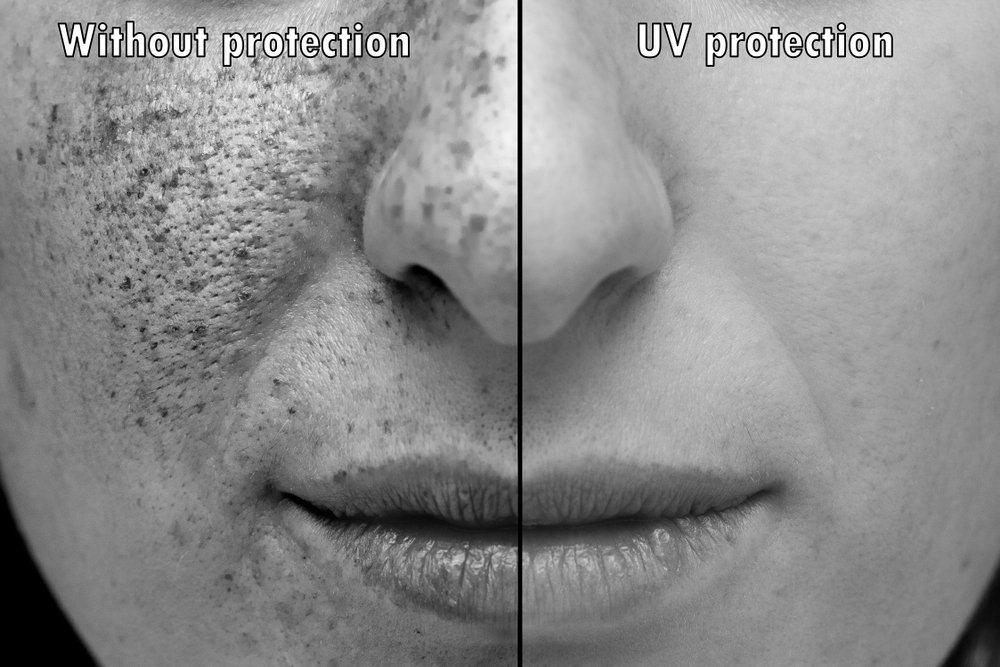
Ultraviolet (UV) light from the sun is the main cause of skin cancers. Cumulative sun damage to the skin causes cosmetic changes that prematurely age skin but also more worrisome DNA changes that can lead to these skin cancers.
When confronted with a new skin cancer diagnosis, patients are often fraught with numerous concerns. These concerns can heighten when the lesion is on their face, with possible disfigurement weighing heavily on patients’ minds.
Despite their high prevalence, fortunately skin cancers are highly curable when detected early and treated appropriately. Routine skin checks increase the early detection of cancers which leads to higher cure rates.
Skin cancers are treated by multiple modalities depending on the type and extent of the lesion. One of the most common treatments is surgical excision, the goal of which is to remove all of the cancer present. In order to do so, a surgical margin of unaffected tissue around the cancer is also removed to ensure complete excision.
For facial skin cancers, Mohs reconstructive surgery has becoming an increasingly popular treatment. The dermatologic surgeon removes the cancer completely with minimal removal of adjacent unaffected/normal tissue. Mohs surgery has also proven to demonstrate excellent skin cancer cure rates while minimizing morbidity.
More complex Mohs surgery will invariably leave behind a defect after removing the lesion. In many cases, the resulting defect can be repaired by the Mohs surgeon, however when the defect is more extensive, facial plastic surgeons assist with the reconstruction.
There are often multiple ways to repair a surgical defect from a Mohs skin cancer removal, and my role as a facial plastic and reconstructive surgeon is to provide the best repair possible.
When a patient presents with a surgical defect to repair, it can be overwhelming for them to imagine the outcome. A thorough discussion with the patient is imperative to explain the surgical plan and the expected recovery and help them understand the reconstructive process.
For many patients, looking in the mirror after their Mohs surgery can be reminder of the diagnosis and the anxiety that accompanied it. My role as a facial reconstructive surgeon provides an opportunity to help patients get back to their lives, feeling confident and knowing that they look and feel more like themselves.


Leave a Reply